As a Licensed Mental Health Counselor (LMHC) based in Miami, FL, and an active advocate for the LGBTQ+ community, I write with deep concern about recent cuts to statewide and federal services that are disproportionately affecting LGBTQ+ Floridians—especially those in Miami-Dade County. These reductions are not abstract policy shifts; they have visible consequences on mental health and substance use outcomes among those I serve every day.
Ending of LGBTQ‑Specific 988 Hotline Services
The 988 line was a landmark development in mental health support. Anyone in crisis could dial or text 988 to reach trained counselors. Within that system, one could “Press 3” (or text “PRIDE”) to connect directly with LGBTQ+‑specialized listeners—people with lived experience and specialized training The Trevor Project.
Since its pilot in late 2022, this service answered more than 1.3 million contacts from LGBTQ+ youth, with approximately 70,000 calls per month in recent months NAMI+3The Trevor Project+3KFF Health News+3. Nearly half of those contacts were routed through The Trevor Project, which handled around 231,000 crisis interactions in 2024 alone .
However, on July 17, 2025, the LGBTQ+‑specific option (“Press 3” or texting “PRIDE”) on the national 988 Suicide & Crisis Hotline was discontinued. That specialized lifeline connected LGBTQ+ youth with peer-trained counselors—a critical resource that handled over 1.2 million youth contacts since its launch in 2022 Catalyst Miami+2Orlando Weekly+2Florida Policy Institute+2Spectrum News 13.
In Florida—including Miami—this service was a cornerstone of immediate, affirming crisis support. Local organizations such as Zebra Coalition reported that federal cuts jeopardized their ability to train and fund crisis staff, even as demand grew . Youth and families I work with describe that loss as “devastating,” especially in areas where local affirming alternatives are already underfunded.
Why This Matters: Elevated Risks Among LGBTQ+ Youth
Research consistently shows that LGBTQ+ youth face mental health challenges at significantly higher rates than their peers. According to surveys by The Trevor Project, ~40% of LGBTQ+ youth seriously considered suicide in 2023; nearly 10% attempted it . They are also more likely to experience depression, anxiety, and misuse substances—often due to stigma, rejection, or trauma.
Specialized peer‑centered support can make a life‑saving difference. A counselor who understands LGBTQ+ experiences—identity rejection, coming out, or navigating societal pressures—can provide validation that general crisis counselors may lack. This cultural competency builds trust and encourages help‑seeking behaviors.
LGBTQ+ youth are also more likely to self-medicate through drugs or alcohol when struggling with mental health. Without access to affirming, trained listeners, crises can escalate: turning to substances, withdrawing from supports, or contemplating self‑harm.
Substance Use: A Critical Intersection with Mental Health
Clinically, we often see that mental health challenges and substance use are two sides of the same coin. For LGBTQ+ individuals—particularly youth—rates of substance misuse (including alcohol, nicotine, and illicit drugs) are consistently higher due to minority stress: the chronic pressure from societal discrimination and internalized stigma .
Tailored crisis counseling can interrupt this harmful cycle. A therapist who is affirming can address mental health distress directly, reducing the need to self-soothe with substances. Removing these supports undercuts a prevention strategy grounded in lived experience and trust.
Medicaid-Based Gender‑Affirming Care Bans and Barriers
Florida’s Medicaid program has been under attack:
- Since August 21, 2022, the Florida Agency for Health Care Administration (AHCA) enacted rules banning Medicaid coverage for puberty blockers, hormone therapy, and gender-affirming surgeries for both minors and adults AP News+9Politico+9AP News+9.
- A federal court in June 2023 ruled that ban unconstitutional—but Florida continues to impose onerous regulations such as mandatory suicide‑risk screenings, written informed consent, and psychiatric comorbidity exclusions, which effectively limit access .
- These restrictions impact more than 9,000 Medicaid-funded transgender Floridians .
For many LGBTQ+ residents of Miami, especially low-income transgender individuals, this translates to abrupt treatment disruptions, escalating mental health distress, and increased risk for self-medication or relapse.
Withdrawal of Local LGBTQ+ Service Funding
Local nonprofits in Miami-Dade and Central Florida are losing vital resources:
- Organizations like Zebra Coalition in Orlando and others anticipated $750,000 in state support to expand housing for at-risk youth—funding later vetoed by the governor FOX 35 Orlando.
- In Orlando, the LGBT+ Center began a fundraiser (“Journey Forward”) to offset federal and state cutbacks that threaten free mental health counseling, HIV testing, and support programs—services also essential to Miami’s community Orlando Weekly+3Spectrum News 13+3.
- Miami-based Pridelines, which provides mental health counseling, housing case management, healthcare access, and substance use support across Miami-Dade, now faces increased strain as public funding dries up Wikipedia.
These organizations are lifelines for many LGBTQ+ individuals, especially youth and low-income residents who rely on free or sliding-scale services.
Why These Cuts Matter for Mental Health & Substance Use
Elevated Baseline Risks
LGBTQ+ individuals—especially youth—experience:
- Higher rates of depression, anxiety, suicidal ideation, and attempts. In 2023, nearly 40% of LGBTQ+ youth seriously considered suicide .
- Increased likelihood of substance misuse as a coping strategy for minority stress, stigma, and identity-related trauma.
Loss of Trusted, Identity-Affirming Supports
Specialized crisis lines and affirming providers make a difference:
- LGBTQ+ youth feel heard, seen, and validated—factors essential to mental wellness.
- Removing these services pushes young people toward crisis points where substance use may escalate.
Healthcare Disruptions Exacerbate Distress
Interrupted access to gender-affirming care often triggers psychiatric crises:
- Trans clients report abrupt hormone therapy cessation due to insurance refusals.
- Forced delays or complex approval processes increase stress, dysphoria, and feelings of helplessness—sometimes leading to substance misuse to cope.
The Miami Perspective: Real Impacts in Real Communities
Miami-Dade’s LGBTQ+ population is diverse, vibrant—and vulnerable. Many youth without supportive home environments rely on community centers and crisis lines to access safe, affirming care.
Organizations like Pridelines offer comprehensive wraparound services: mental health counseling, meals, housing support, PrEP/PEP/ARV access, and substance use outreach. But with cuts to federal crisis funding, these providers struggle to maintain staff training, clinical capacity, and 24/7 responsiveness.
In therapy, I have encountered teens who felt abandoned when crisis supports disappeared, and families who can no longer afford hormone therapy or supportive medications. The result: increased isolation, elevated hopelessness, and in some cases, substance misuse as self-medication.
My Ethical Commitment: Nonmaleficence, Competence, & Justice
As a licensed clinician, my responsibility is clear:
- Nonmaleficence: Not allowing systemic cuts to harm vulnerable populations.
- Competence: Providing culturally informed, identity-respecting care.
- Social justice: Ensuring equitable access to mental health and substance use treatment.
To LGBTQ+ survivors and community members: you are seen, you are worthy, and you deserve care that honors who you are. While the loss of specialized federal crisis services is painful, we are not powerless. Clinicians, community leaders, advocates, and allies are stepping up to fill the gap—with empathy, commitment, and fierce advocacy.
Final Thoughts
This is not about politics—it’s about people. These cuts put lives at risk. Young people in crisis, those seeking gender-affirming care, and vulnerable LGBTQ+ Floridians deserve more—not less.
But there is also strength in community. Across Miami and beyond, peer organizations, dedicated therapists, and resilient LGBTQ+ individuals continue to create spaces for healing, support, and hope. Even when systems fail, our duty remains: to care, to show up, and to speak out.
If you are reading this and in crisis: you are not invisible. You matter. Please reach out—to trusted clinicians, to local resources, or to peers who understand. Together, we will keep building the affirming world you deserve.



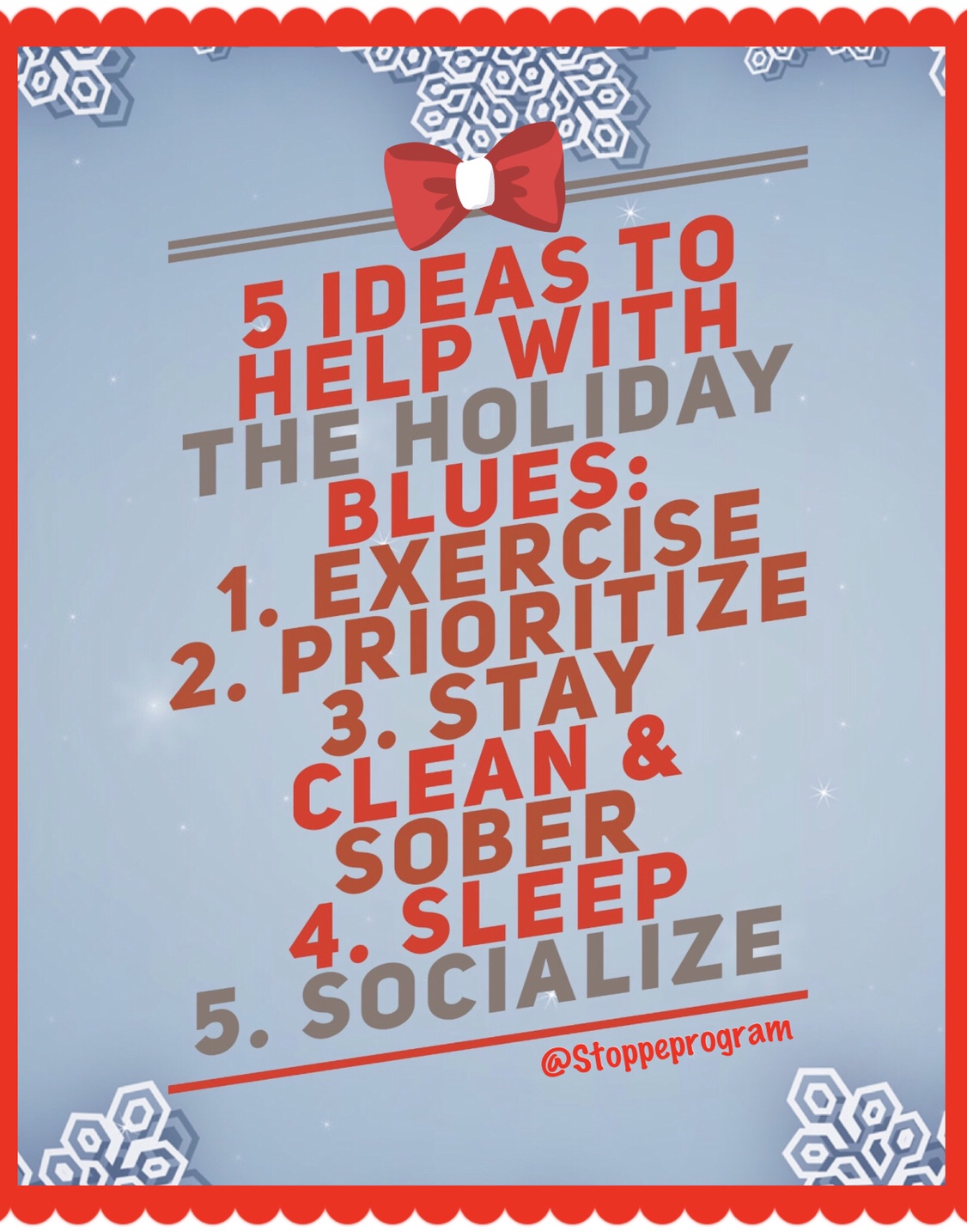 November and December are supposed to be the happiest months of the year, filled with celebration and joy. But are they? For some, stress, unrealistic expectations and even memories surrounding the holidays can trigger feelings of sadness, loneliness and anxiety, commonly known as the “holiday blues.” There’s no way to avoid or circumvent the holiday season, so what can you do?
November and December are supposed to be the happiest months of the year, filled with celebration and joy. But are they? For some, stress, unrealistic expectations and even memories surrounding the holidays can trigger feelings of sadness, loneliness and anxiety, commonly known as the “holiday blues.” There’s no way to avoid or circumvent the holiday season, so what can you do?