Let’s talk about therapy again—because if the last post helped you see that therapy isn’t just for people in crisis, this one will help you take the next step: understanding how it actually works and how it can transform your life, even when things don’t feel “bad enough.”
Whether you’re dealing with anxiety, grief, relationship stress, or substance use, therapy isn’t about fixing what’s broken. It’s about understanding your story, your patterns, and your power to create change.
Therapy Is a Relationship, Not a Fix
At its core, therapy is a relationship between you and your therapist—a space where you’re safe to say things you’ve never said out loud, ask questions you’re afraid to ask, and hear yourself think without being judged.
You’re not being lectured or given advice. You’re being heard, guided, and sometimes challenged gently to grow.
✅ Think of your therapist like a hiking guide—not climbing the mountain for you, but walking beside you, helping you read the map and avoid the cliffs.
What Actually Happens in a Session?
Each therapist has a style, but here’s what a typical session might include:
- Check-in: How have you been feeling since the last session? Any wins or hard moments?
- Processing: You’ll explore thoughts, emotions, or memories in a safe space. This may involve talking through a tough conversation or sitting with a difficult feeling.
- Insight-building: Your therapist may help you notice patterns in your thoughts or behaviors that you didn’t realize were there.
- Skill-building: You might learn tools to manage anxiety, improve communication, or handle cravings.
- Action steps: You’ll often leave with something to reflect on or try during the week.
🧠 Therapy isn’t just venting—it’s intentional, guided, and builds momentum over time.
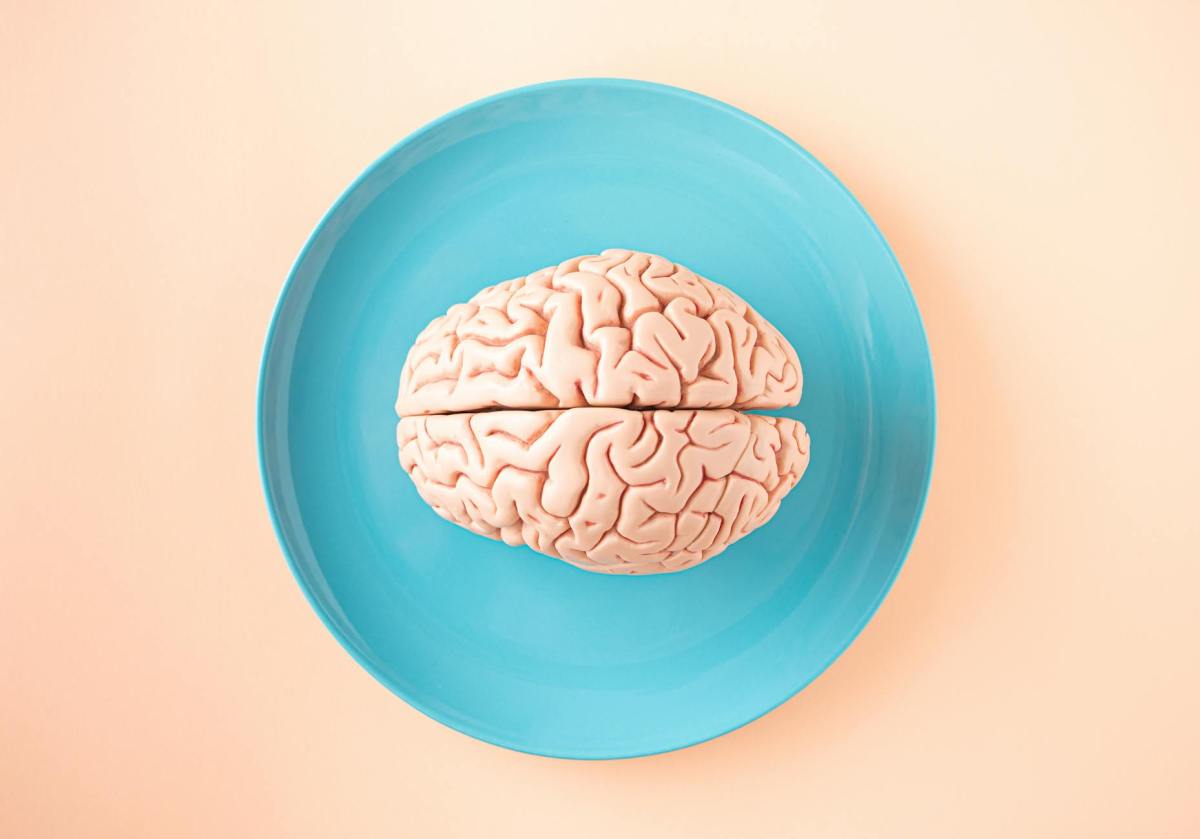
Let’s Talk About CBT (Cognitive Behavioral Therapy)
One of the most commonly used approaches is CBT (Cognitive Behavioral Therapy)—and no, it’s not just a buzzword.
CBT helps you identify how your thoughts, feelings, and behaviors are connected.
Here’s a super simple example:
- Thought: “I always mess up, so why bother trying?”
- Feeling: Hopeless, anxious
- Behavior: You avoid applying for a job or talking to someone new
CBT helps you challenge the thought and replace it with something more helpful:
- New thought: “I’ve made mistakes, but I’ve also learned a lot. I can try again.”
- Feeling: Hopeful, more confident
- Behavior: You take a step forward
💡 CBT gives you tools to rewire your brain, and research shows it’s incredibly effective for anxiety, depression, trauma, and substance use disorders.
What If I Don’t Know Where to Start?
You don’t need to have it all figured out.
Some clients walk into therapy saying, “I don’t know what I need, but I know I need something.” That’s a perfectly fine place to start. In fact, it’s common.
Your therapist might begin by asking:
- What brought you here today?
- What’s one area of life you wish felt better?
- What do you want to understand about yourself?
You’ll set goals together, and those goals can evolve as you grow.
Therapy and Substance Use: Getting to the Root
If you’re in recovery or struggling with substance use, therapy helps you explore the why behind the cravings or behavior.
Instead of focusing just on stopping the behavior, therapy asks:
- What are you trying to cope with?
- What does the substance do for you?
- What are healthier ways to meet those needs?
You may not stop overnight—but therapy offers compassionate accountability. It’s about helping you build a life you don’t want to escape from.
An Example from the Couch
Let’s say Daniel, a 34-year-old father of two, started therapy because he “just felt off.” He said he was tired all the time, didn’t have patience for his kids, and had started drinking more at night to unwind.
In therapy, Daniel realized he had been holding in grief from losing his dad two years ago. He also noticed that when he felt inadequate as a parent, he reached for alcohol.
Through CBT, Daniel learned to recognize his self-critical thoughts and replace them with more compassionate ones. He also started journaling, attending a support group, and setting boundaries around his drinking. Over time, his relationship with his kids improved—and so did his self-respect.
“Therapy didn’t change everything overnight,” he said, “but it gave me my power back.”
What If I’ve Had a Bad Experience in Therapy?
That’s valid. Not every therapist is the right fit, and not every approach works for every person.
But one bad experience doesn’t mean therapy can’t work for you. It might just mean:
- You need a therapist with a different style
- You weren’t ready at the time
- The goals weren’t clearly defined
🌱 Therapy is a process, and finding the right therapist can make all the difference. (Think of it like dating—you may need to try a few before finding “your person.”)
Therapy Is a Tool, Not a Label
Therapy doesn’t mean you’re broken. It means you’re brave enough to want more—for yourself, your relationships, and your future.
📊 According to the American Psychological Association:
- 75% of people who enter therapy show some benefit
- People who engage consistently experience greater emotional resilience and improved relationships
So if you’re wondering if therapy is worth it—the data, and millions of stories, say yes.
Ready to Take the First Step?
You don’t need a diagnosis. You don’t need to be in crisis. You don’t need to have the right words.
You just need a willingness to show up for yourself.
Therapy is your time, your story, and your journey. And you don’t have to do it alone.
💬 Tell Me: What’s Stopped You from Trying Therapy in the Past?
Leave a comment below and let’s normalize the conversation together.
🧠💛 You’re not broken. You’re growing. And therapy can help.