Hope and Healing: What AA Means by a “Spiritual Experience” (Without Religion)
For many people struggling with substance use, one phrase in the AA Big Book can feel intimidating or even alienating:
“You must have a spiritual experience to recover.”
If you’ve ever thought:
- “I’m not religious.”
- “I’ve been hurt by religion.”
- “I don’t believe in God.”
- “This isn’t for me.”
You are not alone—and you are not excluded from recovery.
As a licensed mental health counselor working in substance use treatment, I hear this concern often. The good news is this: AA’s concept of a spiritual experience is far broader, more flexible, and more psychologically grounded than many people realize.
In this blog, we’ll explore what the Big Book actually means by “spiritual experience,” how it connects to modern mental health science, and why it’s really about hope, healing, and internal change—not religion.
Why the Word “Spiritual” Can Feel So Loaded
For many clients, the word spiritual brings up strong emotions. These reactions are valid.
People may associate spirituality with:
- rigid belief systems
- shame or fear-based teachings
- exclusion or judgment
- past trauma
- pressure to believe something that doesn’t feel authentic
So when AA uses spiritual language, it can feel like another barrier instead of a solution.
But here’s the key clarification:
AA does not require religion, belief in God, or adherence to doctrine.
The Big Book explicitly states that spirituality is personal, flexible, and self-defined.
What the Big Book Actually Means by a “Spiritual Experience”
In AA terms, a spiritual experience is an internal shift—not a supernatural event.
The Big Book describes it as:
- a change in attitude
- a new way of thinking
- a shift in values
- a sense of connection
- relief from mental obsession
- freedom from constant self-centered fear
In therapy, we might call this:
- cognitive restructuring
- emotional regulation
- identity transformation
- nervous system stabilization
- meaning-making
- post-traumatic growth
Different words—same process.
Two Types of Spiritual Experiences (According to AA)
The Big Book describes two forms of spiritual experience:
1. The Sudden Change
This is the “aha moment”—a dramatic internal shift where cravings disappear quickly. While powerful, this is not the norm.
2. The Educational or Gradual Change
This is far more common and deeply therapeutic. It happens slowly through:
- insight
- self-awareness
- support
- consistency
- connection
- honesty
Most clients experience recovery this way—and it is just as valid.
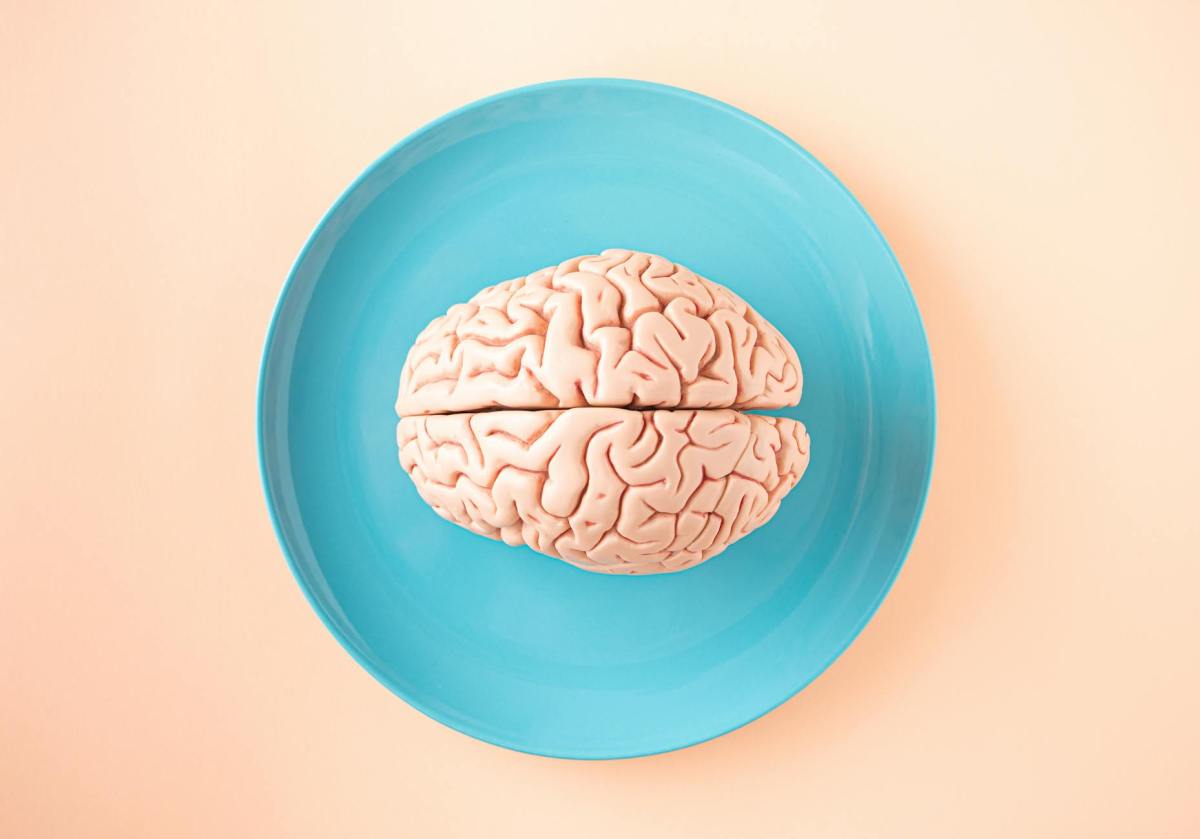
From a Clinical Lens: What’s Really Happening
When someone experiences a “spiritual awakening,” several psychological processes are often occurring:
✅ The nervous system calms
Substances are no longer needed to regulate overwhelming emotions.
✅ The brain learns new coping pathways
The person begins responding instead of reacting.
✅ The internal narrative changes
“I’m broken” becomes “I’m learning.”
✅ Connection replaces isolation
Healing happens in relationship—with people, values, or purpose.
✅ Hope becomes sustainable
Life begins to feel tolerable—and eventually meaningful—without substances.
This is not religious.
It is human healing.
Client Example: A Spiritual Experience Without Religion
Alex, a 38-year-old client, came into treatment adamantly against AA:
“I don’t believe in God. This isn’t for me.”
Over time, Alex stopped fighting the word spiritual and redefined it:
- honesty instead of denial
- connection instead of isolation
- accountability instead of shame
- values instead of avoidance
One day Alex said:
“I still don’t believe in God—but I don’t feel empty anymore.”
That was the spiritual experience.
You Get to Define What Spirituality Means to You
AA encourages people to define spirituality on their own terms.
Some non-religious examples include:
- connection to nature
- belief in humanity
- commitment to values
- mindfulness
- service to others
- inner peace
- curiosity
- personal growth
- compassion
Spirituality in recovery simply means:
something greater than the addiction.
Therapy + AA: Translating Spiritual Language Into Practical Healing
In counseling, we often help clients translate AA concepts into accessible tools:
🔹 “Higher Power”
→ support system, values, recovery community, internal wisdom
🔹 “Spiritual awakening”
→ emotional and cognitive growth
🔹 “Letting go”
→ reducing control, perfectionism, and self-blame
🔹 “Faith”
→ willingness to try something new, even without certainty
This translation helps clients stay engaged instead of feeling alienated.
Reflection Questions for Readers
If spirituality feels uncomfortable, consider these questions:
- What helps me feel grounded?
- When do I feel most connected?
- What values matter to me now?
- What helps me tolerate discomfort without using?
- What would hope look like in my life?
There are no right answers—only honest ones.
Why This Concept Matters for Long-Term Recovery
Substances often fill a void:
- emotional
- relational
- existential
A spiritual experience doesn’t “fix” everything—but it creates space.
Space to:
- feel emotions
- build meaning
- tolerate uncertainty
- experience joy
- live intentionally
Without that internal shift, sobriety can feel like deprivation.
With it, recovery becomes expansion.
Final Thoughts: You’re Not Being Asked to Believe—You’re Being Invited to Heal
AA does not ask you to adopt religion.
It asks you to stay open.
A spiritual experience in recovery is:
- personal
- gradual
- grounded
- human
- healing
If you’ve avoided AA because of the word spiritual, know this:
There is room for you here—exactly as you are.